Anal Fissure Treatment
Gentle & Effective Healing at Siyaram Hospital
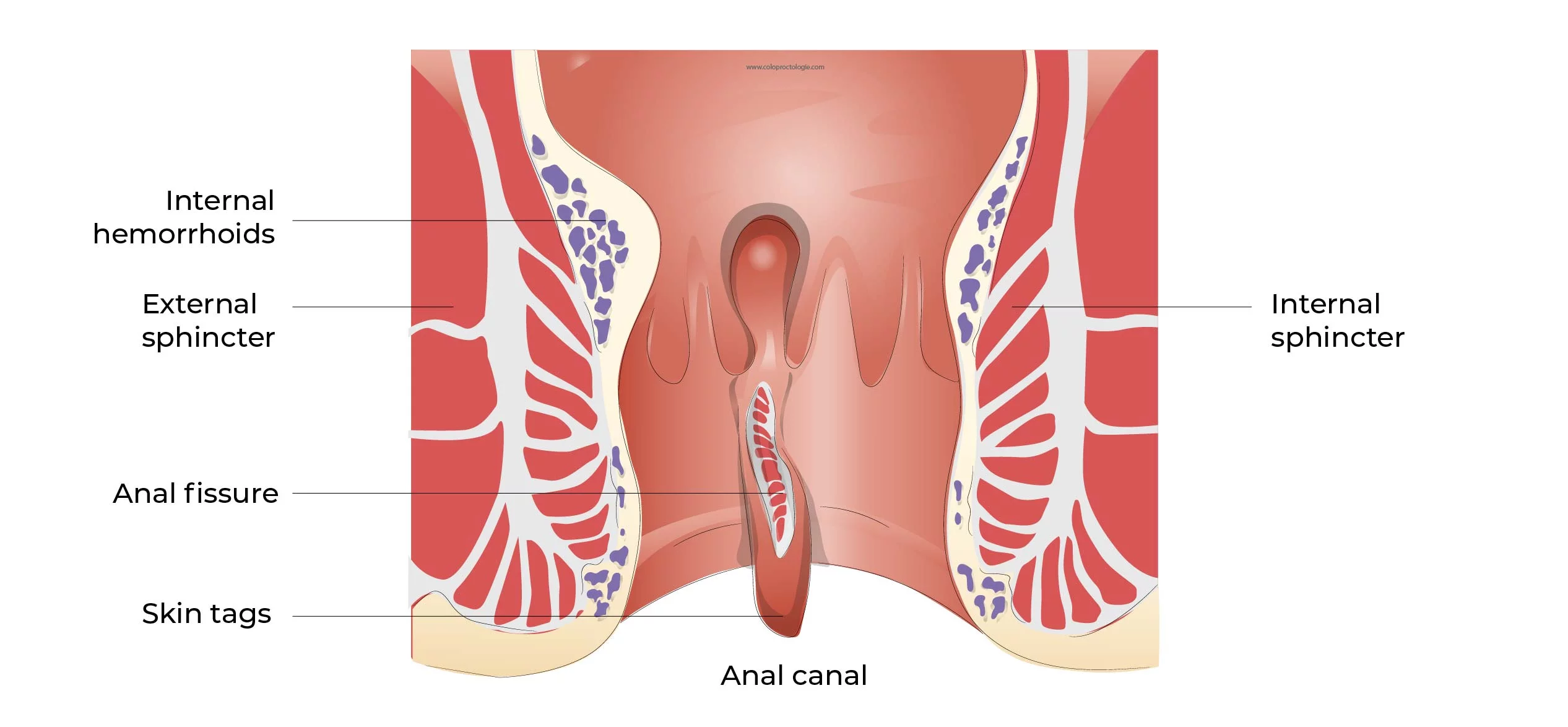
What is an Anal Fissure?
An anal fissure is a small tear in the lining of the anus that causes sharp pain and occasional bleeding during bowel movements. At Siyaram Hospital, we specialize in non-surgical and minimally invasive treatments that help heal fissures effectively, restoring comfort and peace of mind.
Common Symptoms
- Sharp or burning pain during or after bowel movements
- Bright red blood on toilet paper or in stool
- Itching or irritation around the anus
- Visible tear or crack near the anus
- Discomfort when sitting for long periods
Diagnosis at Siyaram Hospital
Our specialists conduct a gentle physical examination and may perform a digital rectal exam. In some cases, an anoscopy (a small, lighted scope) is used for a closer look. If the area is too painful, a topical anesthetic is applied to keep you comfortable during the diagnosis.
Anal Fissure Treatment Options
Topical Anaesthetics
Lidocaine ointment is applied to numb the area before passing stool. This provides fast relief and helps the fissure start healing.
GTN Ointment
Glyceryl trinitrate (GTN) helps relax the muscle and increase blood flow to promote healing. Applied directly twice daily.
Calcium Channel Blockers
For patients who can’t use GTN, these medicines relax the muscle and reduce pain and spasms effectively.
Botox Injection
A modern solution for chronic fissures. Botox helps relax the sphincter muscle and allows the tear to heal naturally.
Post-Treatment Recovery
Most fissures heal within 4–8 weeks with proper care. At Siyaram Hospital, we recommend staying hydrated, eating a fiber-rich diet, and using stool softeners if needed. Our care team provides clear aftercare instructions to minimize discomfort and ensure faster recovery.
Contact Siyaram Hospital If You Notice:
- Persistent or worsening pain
- Heavy rectal bleeding
- Signs of infection or fever
- Difficulty passing stool or urine
Concerned About Anal Fissure?
Speak with our team at Siyaram Hospital today. Fast, confidential advice is just a click away.
Chat on WhatsApp