- contact@siyaramhospitals.com
- By-Pass Road, Tikait Nagar, Uttar Pradesh 225415
- Open 24/7 for all your healthcare needs
Notice: For Emergencies, please call +91-8381308083. Our team available to assist you 24/7.Get More Info

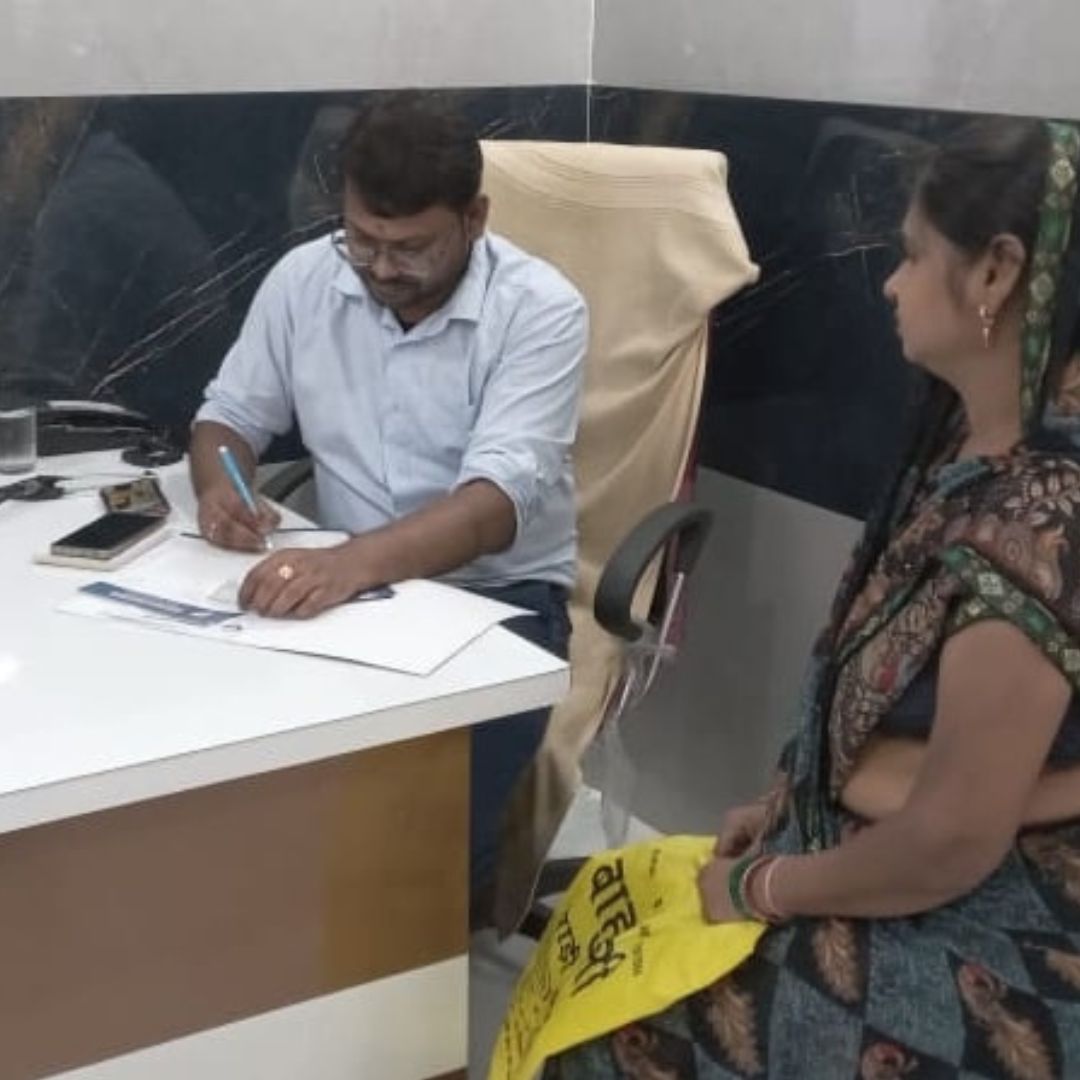
At Siyaram Hospital, we provide personalized medical solutions to enhance patient health and well-being, delivered by skilled professionals using advanced medical technology.
Visiting Hours
| Mon - Fri: | 8:00 am - 8:00 pm |
| Saturday: | 9:00 am - 6:00 pm |
| Sunday: | 9:00 am - 6:00 pm |
Gallery Posts